
Diabetes mellitus is a common disease that, perhaps, all adults have heard of. It can be congenital or acquired during life, but in any case it is chronic and cannot be completely cured. Many have heard that diabetes is not a disease, but a way of life. After all, the patient must follow a special diet for life and use individually selected drugs, and not always insulin injections. In general, nutrition in diabetes mellitus cannot be considered a diet in the generalized sense of the word, because there are not so many restrictions and most of the prohibited products can be replaced with similar taste properties, but safe for the sensitive body. of a diabetic.
What is diabetes mellitus and its types?
Diabetes mellitus is a chronic disease in which there is a violation of glucose metabolism. It can be a consequence of a decrease in the amount of the hormone insulin produced by the cells of the pancreas, then type 1 diabetes mellitus (insulin dependent) is diagnosed or it becomes the result of regular overeating leading to obesity, severe stress and other factors, then type 2 diabetes mellitus (non-insulin dependent) develops.
Insulin is a biologically active substance that is released into the blood, captures a glucose molecule and transports it to the desired cells.
It is type 2 diabetes that is diagnosed most frequently today and requires greater attention from doctors, as well as compliance with special principles of nutrition, since it becomes a consequence of the unhealthy lifestyle that carries a person. With the regular intake of a large amount of carbohydrates in the body, the pancreas works for wear and tear and eventually stops coping with its function or produces "damaged" insulin, which cells and tissues do not perceive. This means that said insulin is unable to capture glucose and transport it to its destination, since the cells "do not see" it, that is. develops insensitivity to it. The changes in the hormonal background that inevitably arise with age play an important role in this.
In both cases, there will be a sharp increase in the concentration of glucose (sugar) in the blood and the development of characteristic symptoms:
- increased thirst;
- dry mouth;
- weakness;
- vision impairment;
- increased appetite, etc.
Type 2 diabetes mellitus is diagnosed more frequently, that is, in 85-90% of patients. It usually occurs after age 40 and especially often after age 65. Such susceptibility of the elderly to the development of carbohydrate metabolism disorders is a consequence of a decrease in physical activity and a decrease in muscle mass, which is the main consumer of glucose, and abdominal obesity is increasingly observed. becoming an additional factor that increases the risk of developing non-insulin dependent diabetes.
Abdominal obesity is the predominant deposit of adipose tissue in the abdomen.
Diagnosing diabetes is not difficult. To do this, a blood glucose test is performed. Obtaining increased indicators serves as the reason for a more detailed examination and selection of optimal treatment tactics, one of the mandatory components of which is nutritional correction.
Why it is important to follow basic nutritional principles
With any type of diabetes mellitus, the blood sugar level rises, but despite this, the cells cannot receive it due to insulin deficiency or the development of insulin resistance. Since glucose is a monosaccharide product of the breakdown of carbohydrates, it acts as the body's main source of energy. Therefore, if the tissues do not receive it in sufficient quantities, they experience hunger, which, due to the transmission of corresponding nerve impulses to the brain, leads to the appearance of a similar sensation in humans. Therefore, with diabetes, patients may feel like eating something, especially sweet, even an hour after a large meal.
As a result, patients overeat foods high in carbohydrate calories, which in type 2 diabetes mellitus rapidly leads to weight gain and the progression of obesity. This leads to an even greater jump in blood glucose levels, an increase in the load on the pancreas, an increase in insulin production, an increase in tissue resistance, a worsening of the condition, i. e. the formation of a vicious vicious cycle.

In such situations, if you don't intervene in a timely manner and break this cycle, high blood sugar (hyperglycemia) will lead to the development of ketoacidosis and diabetic coma. Initially, the patient will feel a strong thirst and often go to the bathroom, then weakness will quickly join, shortness of breath, a characteristic smell of acetone from the mouth and urine will appear, nausea and vomiting will occur. In the absence of competent medical care, confusion and ultimately a diabetic coma will ensue.
In addition, long-term (decompensated) uncontrolled diabetes mellitus can lead to the development of:
- retinal lesions with subsequent irreversible blindness;
- impaired kidney function and chronic kidney failure;
- trophic leg ulcers that heal poorly, very difficult to treat;
- osteoporosis, fraught with the possibility of fracture of any of the bones of the skeleton, including the spine, even with a minor impact;
- disorders of the heart and blood vessels, organs of the digestive tract, etc.
Therefore, it is important not only to diagnose diabetes mellitus in time and to take the drugs prescribed by the endocrinologist, but also to strictly follow the recommendations regarding nutrition.
Diet characteristics
The diet for type 1 and type 2 diabetes mellitus has some differences that patients should understand. With regard to nutrition for insulin-dependent diabetes, in which patients receive lifelong replacement therapy in the form of regular insulin injections, doctors in different countries discuss the need to limit simple carbohydrates in different ways.
Foreign endocrinologists believe that it is not necessary to reduce the amount of your intake in type 1 diabetes with properly selected insulin therapy. Domestic doctors believe that this is fraught with undesirable consequences and insist on the need to limit the consumption of simple carbohydrates, but not to abandon them completely, as in non-insulin-dependent diabetes. In type 2 diabetes mellitus, such disputes are inappropriate, since with it the use of sugar can turn into dire consequences, which is not questioned in any country.
Also, people with type 1 diabetes should be able to count bread units (XE) and people with type 2 diabetes should be able to determine the glycemic index (GI). Nutrition should be structured in such a way that these indicators of the daily diet correspond to the developed norms.
Therefore, today with diabetes mellitus, patients are prescribed the so-called diet No. 9 in various modifications, the differences of which are insignificant. The endocrinologist determines which table is best suited for a particular patient, based on the results of the tests and the person's condition.
In general, Diet No. 9 is designed in such a way that it normalizes carbohydrate metabolism by reducing the amount of simple carbohydrates consumed and consequently lowering the level of glucose in the blood. As a result, it is possible to normalize the amount of sugar in the blood, prevent the development of possible disorders of fat metabolism and complications of the disease.
Diet No. 9 assumes a complete rejection of simple carbohydrates in the context of daily consumption of no more than 300 g of complex carbohydrates while keeping the amount of protein foods within the physiological norm.
Basic nutritional principles
In case of diabetes mellitus of any type, the following recommendations should be observed:
- the meal must certainly be fractional and consist of at least 5 meals, especially with an insulin-dependent form;
- breakfast is a mandatory meal;
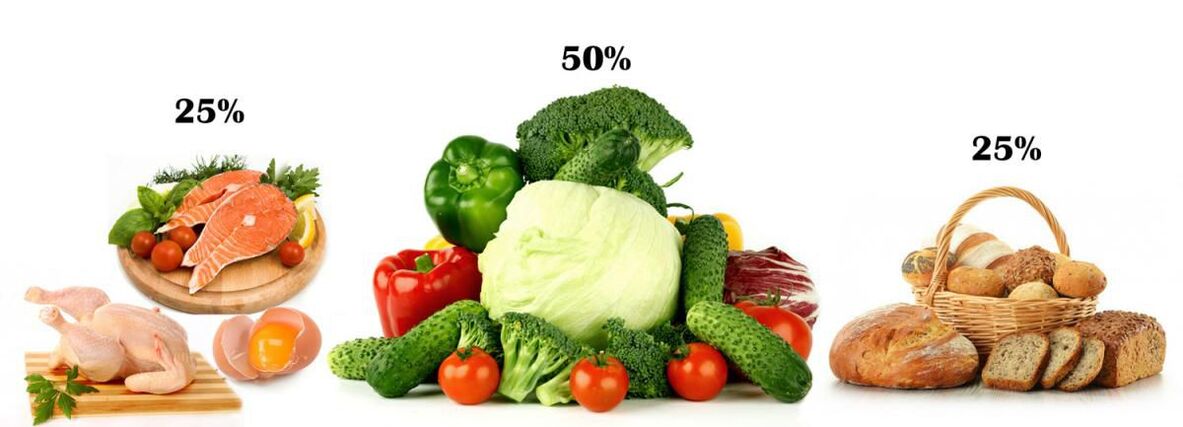
- When preparing the menu, the physiological proportion of proteins (meat, fish dishes, dairy products), carbohydrates (cereals, bread) and vegetables must be respected, which must represent 25%, 25% and 50%, respectively;
- The nutritional advantage is always given to foods with a low glycemic index and a high percentage of vegetable fiber;
- each meal begins with vegetables and proteins are left at the end;
- the amount of salt should not exceed 5 g per day;
- fasting for diabetes is prohibited, if necessary, to reduce weight, this is done by increasing physical activity;
- when choosing a method of cooking vegetables, it is recommended to give preference to minimal heat treatment or to abandon it altogether, the ideal is to boil, bake and steam;
- A vegetarian diet for diabetes is not the best option, although it helps to improve the course of the disease and increase insulin sensitivity, you can switch to it only with the permission of an endocrinologist.
Nutrition for type 1 diabetes
Insulin-dependent diabetes is usually diagnosed in childhood. Since the cause of its development is the destruction of the cells of the pancreas that synthesize insulin, patients should be prescribed insulin therapy, and the drug and dosage are selected individually. Insulin injections completely cover the deficit in the production of the hormone in the body, so no significant dietary restrictions are required, but the child's parents, and then himself, must learn to correctly calculate the amount of carbohydrates consumed in order to corresponding to the insulin dose administered. For this, tables have been created especially indicating the number of so-called grain units in each product.
In type 1 diabetes mellitus, it is necessary to reject only:
- any sugary drink, including juices;
- prepared breakfast cereals;
- confectionery.
You cannot eat more than XE 7 per meal and up to XE 25 per day. In this case, the amount of all carbohydrates eaten per serving volume is added. For example, 2 XE is contained in 3 tablespoons. l. finished pasta, 4 tbsp. l. rice, 14 tbsp. l. legumes or 420 g of tomatoes.
1 XE equals 12g of carbohydrates or 20g of bread.
Sweets are not strictly prohibited, but only those who monitor the level of glucose in the blood several times a day can afford it, they have XE precision and can independently regulate the dose of insulin administered.
In severe type 1 diabetes mellitus, patients are prescribed diet # 9b and large doses of insulin. It involves the use of 400-450g of carbohydrates and is very close to the diet of most modern people. It is allowed to consume 20-30 g of sugar per day.
The endocrinologist who is monitoring the patient's condition will definitely tell you how to distribute the amount of food between individual doses, depending on the type of medication that he has prescribed. So, with the introduction of insulin twice a day (in the morning and in the evening), it is necessary to compose the menu so that almost 2/3 of the total daily carbohydrate intake falls at this time. Also, after each injection, you need to eat 2 times: 15 minutes after the injection and 3 hours after that. Fractional nutrition and controlling the amount of XE are the foundation of the type 1 diabetes diet.
If, after the injection, the patient suddenly feels weak, this indicates a deficiency of glucose in the body. In such situations, he should immediately eat a piece of dark chocolate.
Thus, with an insulin-dependent form of the disease, the main difficulty lies in the need to control not the type of food, but its volume and to count the units of bread.
Nutrition for type 2 diabetes
In most cases, obesity is the main cause of the disease. Therefore, the diet for type 2 diabetes is the first and main component of the treatment and prevention of complications. With their help, it will be possible to normalize sugar levels and control weight, thus preventing the appearance of unwanted changes and deterioration of the condition.
All patients should independently monitor their blood glucose levels on a daily basis using home glucometers, and if stable high rates are obtained, immediately consult a physician.
If the patient is diagnosed with an insulin-dependent form of the disease of mild or moderate degree and the weight of it is within the normal range, the basic diet No. 9 is assigned with a daily caloric intake of up to 2500 kcal. In such situations, you cannot consume more than 275-300g of complex carbohydrates from different sources per day.
In the presence of obesity, it is required not only to maintain the glucose level within the normal range, but also to reduce weight, since its excess negatively affects the effectiveness of treatment and the well-being of patients. Therefore, in such cases, patients are prescribed the so-called reduced diet No. 9, which is characterized by a reduced caloric content due to an even greater restriction of the permissible amount of complex carbohydrates consumed daily. In this case, the endocrinologist individually calculates this rate based on the degree of obesity. Therefore, in different cases, patients can be allowed to consume 100 to 225 g of carbohydrates, and the total calorie intake should not exceed 1700 kcal per day.
What is not allowed
So, with type 2 diabetes mellitus, it is necessary to completely exclude from the diet foods that contain so-called fast carbohydrates, that is, those that are broken down into glucose and absorbed into the bloodstream within 15 minutes. They quickly give an energy boost, but don't create a feeling of fullness, so after eating them, hunger returns very quickly. These include:
- sugar;
- Dear;
- confectionery, classic pastry;
- chocolate ice cream;
- jam, jam, jam, preserves;
- sweet vegetables, fruits, berries (grapes, bananas, dates, pineapple, persimmon, nuts);
- white bread, loaf;
- semolina;
- smoked meats, fatty dishes;
- Mayonnaise;
- fast food, snacks.
For diabetics, special recipes, including allowed products, have been created for baking.
Diet number 9 does not require a complete refusal, but recommends minimizing the amount consumed as much as possible:
- potatoes;
- beet
- corn;
- carrots;
- soy products;
- pasta;
- of bread.
If you are obese, you will need to completely abandon all high-fat foods:
- butter and vegetable oil for spreading;
- sour cream, fatty cheeses, cottage cheese, cream;
- lard, fatty meats and fish, chicken with skin;
- walnut seeds;
- alcohol, etc.
In such situations, it is recommended to replace these products with vegetables that have a beneficial effect on carbohydrate metabolism. These are green leafy vegetables, eggplants, cucumbers, turnips, cauliflower, squash, zucchini, radishes, etc.
It is imperative to try to completely abandon foods with a large amount of fat, in particular canned foods, products from the meat industry, sauces from the store. They are replaced by boiled or stewed dietary meat (chicken, rabbit, turkey, skimmed yogurt without additives).
Which can
Carbohydrates are an indispensable part of the daily diet and should be present on the menu for diabetes, but only in acceptable amounts. Patients may eat only foods with slow-absorbing, high-fiber carbohydrates. That:
- vegetables;
- whole wheat bread with bran;
- whole grains (8-10 tablespoons), except for refined rice.
Since sugar in any form is prohibited for diabetics, its substitutes that do not contain glucose have been specially created. Many of them are much sweeter than sugar and can be used in trace amounts. Modern sweeteners include xylitol, stevia, sorbitol, fructose. But studies have shown that some of them can have a negative effect on the body. Stevia is considered the safest sugar substitute today. It is obtained from natural raw materials and in sweetness it surpasses sugar between 10 and 30 times (depending on the form of release: a powder of an herb or an extract called stevioside).

It is important for patients to know the glycemic index of foods. Today, there are special tables that help you navigate the choice and correctly calculate the allowable consumption rate. In diabetes, preference should be given to foods with a GI lower than 55 (apples, cucumbers, cherries, broccoli, lettuce, milk, cauliflower, etc. ). They break down slowly and cause little or no increase in blood sugar levels. These products can be consumed up to 200 g during a meal, but preferably together with protein foods.
Heat treatment increases the GI.
It is allowed to use:
- potatoes (no more than 200 g per day);
- dishes based on meat and vegetable broth;
- lean meats and fish (chicken, turkey, haddock, pike, hake);
- lentils
- low-fat fermented milk and milk products, cheeses with a fat content of less than 30%;
- eggs (3-4 per week, but no more than 1 per day);
- vegetable oil (no more than 1 tbsp. l. per day);
- special sweets, waffles, diabetic breads.
When making homemade compotes, sweeteners are added instead of sugar.
Nutrition for gestational diabetes
Pregnant women with a genetic predisposition to the development of diabetes mellitus may face the development of so-called gestational diabetes at 20-24 weeks. It arises against the background of the presence of a hereditary reduced sensitivity of tissues to inulin, amplified by hormones produced during pregnancy in increased amounts: estrogen, prolactin, cortisol. They are able to block insulin and cause blood sugar to rise.
Often after childbirth, carbohydrate metabolism gradually returns to normal, as the hormonal background normalizes. However, if the basic principles of nutrition and diet are not followed, there is not only a risk of preserving diabetes mellitus, but also the development of complications that can lead to premature birth, pyelonephritis in the mother, underlying pathologies. of eye, as well as complications during childbirth. In order to timely detect gestational diabetes during pregnancy, blood glucose tests are regularly performed, and if hyperglycemia is detected, a diet is prescribed.
In such situations, women are advised to:
- completely exclude simple carbohydrates from the diet (the same sugar, confectionery, chocolate, cakes, black and white bread, bananas, grapes, juices, nuts, etc. );
- limit the intake of complex carbohydrates to the amounts recommended by the doctor;
- eliminate most of the daily diet of vegetables, fruits without sugar;
- refuse to eat fatty foods, fried foods, semi-finished products, a variety of sausages, smoked products;
- when choosing a method of cooking products, give preference to baking, stewing, steaming;
- eat divided, preferably every 2 hours, highlighting 3 main meals (breakfast, lunch and dinner), as well as 2 additional (second breakfast, snack);
- Drink at least 1. 5 liters of water.
Pregnant women with gestational diabetes are advised to check their blood sugar after each meal.

All of these recommendations are relevant to the postpartum. In any case, in the first months of a baby's life, a breastfeeding woman is forced to follow a hypoallergenic diet and refuse fried fatty foods. The same diet will help eliminate gestational diabetes and prevent its transition to a chronic carbohydrate metabolism disorder within 2-3 months after delivery. If, after this period of time, the blood glucose level does not return to normal, the woman should consult an endocrinologist to examine and develop treatment tactics.
Sugar reducing products
There are several foods that can help lower blood glucose levels. They are called hypoglycemic agents and are recommended for patients with diabetes mellitus. But since each person is a unique biological system and has individual characteristics, they can react to certain types of food in her own way, and not just give allergic reactions. Therefore, although hypoglycemic foods can provide invaluable help to patients with diabetes mellitus, especially type 2, it is advisable to consult an endocrinologist before starting their daily use.
So foods that reduce sugar include:
- Cherries (GI 22): contains anthocyanin, which helps lower blood sugar and blood pressure, and eliminates so-called bad cholesterol. The daily norm is 100 g.
- Grapefruit (GI 29): contains naringin, a powerful antioxidant that helps increase insulin sensitivity in tissues. It is recommended to consume 1 medium grapefruit or freshly squeezed juice per day (commercial not suitable). But grapefruit can negatively affect the absorption quality of various medications, so it is necessary to consult with your doctor before including it in the menu.
- Cinnamon is a source of polyphenols that help keep blood sugar levels under control. The daily rate is 1/2 tsp. It can be added to cottage cheese, oatmeal and is very suitable for making apple stews.
- Broccoli is a valuable source of fiber, which is very beneficial for diabetes, and the substances it contains help reduce the rate of absorption of sugar in the intestine. The daily norm is 200 g.
- Blueberries are one of the healthiest foods for diabetics, as they contain valuable glycosides, tannins, and anthocyanins, which help maintain normal glucose levels and reduce the risk of developing diabetic retinal damage. The daily norm is 200 g.
- Oatmeal and millet porridge are rich in fiber, which helps maintain sugar levels.
- Jerusalem artichoke is a natural source of insulin, so its use contributes to the normalization of glucose levels, and the presence of fructose in the composition provides a pleasant sweet taste, which allows its use raw or added to salads.
- Garlic is one of the healthiest foods for everyone, as it contains many antioxidants, natural antibacterials, and other substances. Its use makes the pancreas work more actively, which is very valuable for patients with type 1 diabetes.
- Fish: Diabetics with fish have been shown to eat at least 2 times a week and, whenever possible, try to replace meat dishes with it. It helps to normalize sugar levels as well as to obtain essential polyunsaturated fatty acids.

Therefore, nutrition for diabetes mellitus can be varied and tasty. With a competent approach to planning the menu, you will not cause rejection, but, on the contrary, will help to increase energy and efficiency, since it largely corresponds to the principles of rational nutrition. But remember, in diabetes it is important to maintain a normal level of physical activity, since exercise increases the sensitivity of the tissue to insulin.

































